What is Bronchiectasis?
Diagnosed with Bronchiectasis? Always remember that you're not alone. There's lots of help and information out there and you can start right here.

In 2012 around 210,000 people in the UK were living with bronchiectasis and the number increases year on year. Being diagnosed with the condition is more likely for adults between the ages of 30 and 70. If it does occur in children it can be caused by a combination of the genes your child is born with, infections, passive smoking, air pollution or diet and nutrition. If you’re worried about your child contact The British Lung Foundation by clicking here.
Healthy lungs
When you breathe, air is carried into your lungs through your airways (bronchi) These divide again and again into thousands of smaller airways called bronchioles. Your airways contain tiny glands that produce a small amount of mucus. This mucus helps to keep your airways moist, and traps the dust and germs that you breathe in. Normally mucus is moved away by tiny hairs called cilia.
What is Bronchiectasis?
When you have bronchiectasis, your airways are scarred and inflamed with thick mucus. Your airways become widened and cannot clear themselves properly. Pockets in the airways means that mucus builds up and gets trapped, it is likely to get infected leading on to a chest infection or a flare-up of your symptoms. It’s important to recognise and treat chest infections. If you don’t get treatment, your airways may be damaged further. The scarring around your airways can’t be reversed, but there are ways you and your health care team can treat and manage bronchiectasis.
Symptoms of Bronchiectasis
The most common symptom is coughing up sputum or phlegm and for people with more severe bronchiectasis it can be quite a large amount. Frequent chest infections are also a common feature of bronchiectasis. Other symptoms you might have are tiredness, difficulty concentrating, breathlessness, sinus problems, cough incontinence called bladder leakage, anxiety or depression. Symptoms which are less common are coughing up blood, chest pain or joint pain.
How is it diagnosed?
If you develop a persistent cough you should see your GP so they can look for a possible cause. Your GP will ask you about your symptoms, such as how often you cough, whether you bring up any phlegm (sputum) and whether you smoke.
They may also listen to your lungs with a stethoscope as the lungs of people with bronchiectasis often make a distinctive crackling noise as a person breaths in and out. You may need a chest X-ray to rule out other causes of your symptoms and if your GP thinks you may have a lung infection they may take a sample of your phlegm so it can be checked for bacteria.
How is Bronchiectasis treated?
The damage to your lungs from bronchiectasis is permanent but treatment can help prevent the condition getting worse. In most cases, treatment involves a combination of medication, exercises you can learn and devices to help clear your airways.
Surgery for Bronchiectasis is rare and there are lots of things you can do to help yourself such as stop smoking (if you smoke). It’s a good idea to check you’ve had the pneumococcal vaccine and make sure you have the flu jab every year. Regular exercise, a well balanced diet and keeping hydrated also help.
Exercises for your airways
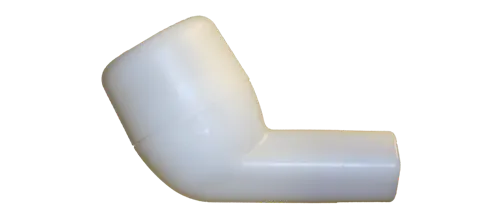
Airway clearance techniques can help to remove mucus from your lungs and these can often help improve coughing and breathlessness. Physiotherapists can teach you ABCT (active cycle breathing technique) and completing the cycle once or twice a day may improve your lung function. Postural drainage can also help making it easier to cough up any mucus. You may be recommended to buy a mucus clearance device such as the Pari O-PEP which uses a combination of vibrations and air pressure to make it easier to cough out any mucus. You can find out more about these devices and how they work by clicking this link.
Medication
Occasionally, medication inhaled through a nebuliser may be recommended to help make it easier for you to clear your lungs. Nebulisers convert your medication into a fine mist which you then breathe in. Our range includes: Philips Nebulisers, Omron Nebulisers, Pari Nebulisers, Medix Nebulisers and Beurer Nebulisers. You can find more information about nebulisers on this blog post: What is a nebuliser?
A saline (salt) solution, normal or hypertonic can help reduce the thickness of your phlegm making it easier for you to cough it out. We've written a bit more detail on our blog post about Nebulising Saline.
Bronchodilators can help make breathing easier by relaxing the muscles in the lungs, or if you have three or more infective exacerbations in any one year you may be prescribed a low dose preventative antibiotic through a nebuliser. Nebulising antibiotics can be a little trickier. Antibiotics should be nebulised through a 'closed system' such as that which is available from Philips Sidestream Plus or Pari filter system. This will protect your nearest and dearest from becoming antibiotic resistant over time. Nebulised antibiotics can also be very sticky so not all nebulisers are suitable. If you are prescribed nebulised medication and are unsure which to choose there’s lots of information in this blog, pages and pages on our website and you can email or call for a chat.
Will I need surgery?
Surgery is usually only recommended where bronchiectasis is only affecting a single section of your lung, your symptoms aren't responding to other treatment and you don't have an underlying condition that could cause bronchiectasis to recur.
How does the future look?
The outlook for people with bronchiectasis is highly variable and often depends on the underlying cause. Living with bronchiectasis can be stressful and frustrating, but most people with the condition have a normal life expectancy. For people with very severe symptoms, however, bronchiectasis can be fatal if the lungs stop working properly. It’s vital to be well informed and up to date with all the help that is available. NHS Choices have lots more reading over on their website and The British Lung Foundation are the experts in helping you look after your lungs providing information, an email contact and a helpline. If you’re newly diagnosed or just not sure what comes next why not take a look?
Photo credits: Lukas Juhas, Alejandro Alvarez, Mikael Häggström